Our phone: 
The circulatory system is an organ system that passes nutrients (such as amino acids and electrolytes), gases, hormones, blood cells, nitrogen waste products, etc. to and from cells in the body to help fight diseases and help stabilize body temperature and pH to maintain homeostasis. This system may be seen strictly as a blood distribution network, but some consider the circulatory system as composed of the cardiovascular system, which distributes blood, and the lymphatic system, which distributes lymph. While humans, as well as other vertebrates, have a closed cardiovascular system (meaning that the blood never leaves the network of arteries, veins and capillaries), some invertebrate groups have an open cardiovascular system. The most primitive animal phyla lack circulatory system. The lymphatic system, on the other hand, is an open system.
The main components of the human circulatory system are the heart, the blood, and the blood vessels. The circulatory system includes: the pulmonary circulation, a "loop" through the lungs where blood is oxygenated; and the systemic circulation, a "loop" through the rest of the body to provide oxygenated blood. An average adult contains five to six quarts (roughly 4.7 to 5.7 liters) of blood, which consists of plasma, red blood cells, white blood cells, and platelets. Also, the digestive system works with the circulatory system to provide the nutrients the system needs to keep the heart pumping.

Two types of fluids move through the circulatory system: blood and lymph. The blood, heart, and blood vessels form the cardiovascular system. The lymph, lymph nodes, and lymph vessels form the lymphatic system. The cardiovascular system and the lymphatic system collectively make up the circulatory system.
Pulmonary circulation is the portion of the cardiovascular system which transports oxygen-depleted blood away from the heart, to the lungs, and returns oxygenated blood back to the heart.
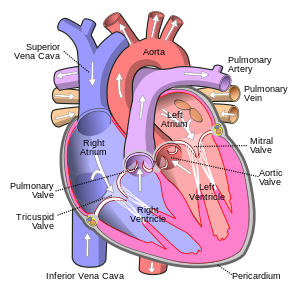
Oxygen deprived blood from the vena cava enters the right atrium of the heart and flows through the tricuspid valve into the right ventricle where it is pumped through the pulmonary semilunar valve into the pulmonary arteries which go to the lungs. Pulmonary veins return the now oxygen-rich blood to the heart, where it enters the left atrium before flowing through the mitral valve into the left ventricle. Also, from the left ventricle the oxygen-rich blood is pumped out via the aorta, and on to the rest of the body.
The heart pumps oxygenated blood to the body and deoxygenated blood to the lungs. In the human heart there is one atrium and one ventricle for each circulation, and with both a systemic and a pulmonary circulation there are four chambers in total: left atrium, left ventricle, right atrium and right ventricle. The right Atrium, which is the upper chamber of the right side. The blood that is returned to the right atrium is deoxygenated (poor in oxygen) and passed into the right ventricle to be pumped through the pulmonary artery to the lungs for re-oxygenation and removal of carbon dioxide. The left atrium receives newly oxygenated blood from the lungs as well as the pulmonary vein which is passed into the strong left ventricle to be pumped through the aorta to the tissues of the body.
Cardiovascular disease or cardiovascular diseases refers to the class of diseases that involve the heart or blood vessels (arteries and veins). While the term technically refers to any disease that affects the cardiovascular system (as used in MeSH), it is usually used to refer to those related to atherosclerosis (arterial disease). These conditions have similar causes, mechanisms, and treatments. In practice, cardiovascular disease is treated by cardiologists, thoracic surgeons, vascular surgeons, neurologists, and interventional radiologists, depending on the organ system that is being treated. There is considerable overlap in the specialties, and it is common for certain procedures to be performed by different types of specialists in the same hospital.
Most countries face high and increasing rates of cardiovascular disease. Each year, heart disease kills more Americans than cancer.
It is the number one cause of death and disability in the United States and most European countries (data available through 2005). A large histological study (PDAY) showed vascular injury accumulates from adolescence, making primary prevention efforts necessary from childhood.
By the time that heart problems are detected, the underlying cause (atherosclerosis) is usually quite advanced, having progressed for decades. There is therefore increased emphasis on preventing atherosclerosis by modifying risk factors, such as healthy eating, exercise and avoidance of smoking.
Hypertension is a chronic medical condition in which the blood pressure is elevated. It is also referred to as high blood pressure or shortened to HT, HTN or HPN. The word "hypertension", by itself, normally refers to systemic, arterial hypertension.
Hypertension can be classified as either essential (primary) or secondary. Essential or primary hypertension means that no medical cause can be found to explain the raised blood pressure. It is common. About 90-95% of hypertension is essential hypertension. Secondary hypertension indicates that the high blood pressure is a result of (i.e., secondary to) another condition, such as kidney disease or tumours (adrenal adenoma or pheochromocytoma).
Persistent hypertension is one of the risk factors for strokes, heart attacks, heart failure and arterial aneurysm, and is a leading cause of chronic renal failure. Even moderate elevation of arterial blood pressure leads to shortened life expectancy. At severely high pressures, defined as mean arterial pressures 50% or more above average, a person can expect to live no more than a few years unless appropriately treated. Beginning at a systolic pressure (which is peak pressure in the arteries, which occurs near the end of the cardiac cycle when the ventricles are contracting) of 115 mmHg and diastolic pressure (which is minimum pressure in the arteries, which occurs near the beginning of the cardiac cycle when the ventricles are filled with blood) of 75 mmHg (commonly written as 115/75 mmHg), cardiovascular disease (CVD) risk doubles for each increment of 20/10 mmHg.
A recent classification recommends blood pressure criteria for defining normal blood pressure, prehypertension, hypertension (stages I and II), and isolated systolic hypertension, which is a common occurrence among the elderly. These readings are based on the average of seated blood pressure readings that were properly measured during 2 or more office visits. In individuals older than 50 years, hypertension is considered to be present when a person's blood pressure is consistently at least 140 mmHg systolic or 90 mmHg diastolic. Patients with blood pressures over 130/80 mmHg along with Type 1 or Type 2 diabetes, or kidney disease require further treatment.
| Classification | Systolic pressure | Diastolic pressure | ||
|---|---|---|---|---|
| mmHg | kPa (kN/m2) | mmHg | kPa (kN/m2) | |
| Normal | 90–119 | 12–15.9 | 60–79 | 8.0–10.5 |
| Prehypertension | 120–139 | 16.0–18.5 | 80–89 | 10.7–11.9 |
| Stage 1 | 140–159 | 18.7–21.2 | 90–99 | 12.0–13.2 |
| Stage 2 | ≥160 | ≥21.3 | ≥100 | ≥13.3 |
| Isolated systolic hypertension | ≥140 | ≥18.7 | <90 | <12.0 |
| Source: American Heart Association (2003). | ||||
Resistant hypertension is defined as the failure to reduce blood pressure to the appropriate level after taking a three-drug regimen (include thiazide diuretic).[8] Guidelines for treating resistant hypertension have been published in the UK, and US.
Excessive elevation in blood pressure during exercise is called exercise hypertension. The upper normal systolic values during exercise reach levels between 200 and 230 mm Hg. Exercise hypertension may be regarded as a precursor to established hypertension at rest.
Lifestyle modifications
Unless hypertension is severe, lifestyle changes such as those discussed in the preceding section are strongly recommended before initiation of drug therapy. Adoption of the DASH diet is one example of lifestyle change repeatedly shown to effectively lower mildly-elevated blood pressure. If hypertension is high enough to justify immediate use of medications, lifestyle changes are initiated concomitantly.
A series of UK guidelines advocate treatment initiation thresholds and desirable targets to be reached as set out in the following table. Of particular note is that for patients with blood pressures between 140-159/80-99 and without additional factors, that only lifestyle actions and regular blood pressure and risk-factor review is proposed.
| Thresholds for starting treatment | Group | Target of treatment |
|---|---|---|
| >160/100 | all those with such persisting readings | <140/90 |
| >140/90 | If also: Cardiovascular risk >20% per 10 years Or have established cardiovascular disease Or have evidence end organ damage Or chronic kidney disease without high levels albuminuria |
<140/90 |
| >130/80 | Type 2 Diabetes alone | <130/80 |
| >135/85 | Type 1 Diabetes alone | <130/80 |
| >130/80 | Type 1 Diabetes with microalbuminuria Or Type 2 Diabetes with kidney, eye or cerebrovascular damage |
<130/80 |
| >130/80 | chronic kidney disease with high levels albuminuria | <125/75 |
Medications
There are many classes of medications for treating hypertension, together called antihypertensives, which — by varying means — act by lowering blood pressure. Evidence suggests that reduction of the blood pressure by 5–6 mmHg can decrease the risk of stroke by 40%, of coronary heart disease by 15–20%, and reduces the likelihood of dementia, heart failure, and mortality from vascular disease.
The aim of treatment should be blood pressure control to <140/90 mmHg for most patients, and lower in certain contexts such as diabetes or kidney disease (some medical professionals recommend keeping levels below 120/80 mmHg). Each added drug may reduce the systolic blood pressure by 5–10 mmHg, so often multiple drugs are often necessary to achieve blood pressure control.
Commonly used drugs include the typical groups of:
Other additionally used groups include:
Finally several agents may be given simultaneously:
Choice of initial medication
Unless the blood pressure is severely elevated, consensus guidelines call for medically-supervised lifestyle changes and observation before recommending initiation of drug therapy. All drug treatments have side effects, and while the evidence of benefit at higher blood pressures is overwhelming, drug trials to lower moderately-elevated blood pressure have failed to reduce overall death rates.
If lifestyle changes are ineffective or the presenting blood pressure is critical, then drug therapy is initiated, often requiring more than one agent to effectively lower hypertension. Which type of many medications should be used initially for hypertension has been the subject of several large studies and various national guidelines.
The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) study showed better cost-effectiveness and slightly better outcomes for the thiazide diuretic chlortalidone compared with a calcium channel blocker and an ACE inhibitor in a 33,357-member ethnically mixed study group. The 1993 consensus recommendation for use of thiazide diuretics as initial treatment stems in part from the ALLHAT study results, which concluded in 2002 that "Thiazide-type diuretics are superior in preventing 1 or more major forms of CVD and are less expensive. They should be preferred for first-step antihypertensive therapy."
A subsequent smaller study (ANBP2) did not show the slight advantages in thiazide diuretic outcomes observed in the ALLHAT study, and actually showed slightly better outcomes for ACE-inhibitors in older white male patients.
Thiazide diuretics are effective, recommended as the best first-line drug for hypertension by many experts, and are much more affordable than other therapies, yet they are not prescribed as often as some newer drugs. Hydrochlorothiazide is perhaps the safest and most inexpensive agent commonly used in this class and is very frequently combined with other agents in a single pill. Doses in excess of 25 milligrams per day of this agent incur an unacceptable risk of low potassium or Hypokalemia. Patients with an exaggerated hypokalemic response to a low dose of a thiazide diuretic should be suspected to have Hyperaldosteronism, a common cause of secondary hypertension.
The consensus recommendations of thiazide diuretics as first-line therapy for hypertension stand against the backdrop that all blood pressure treatments have side-effects. Potentially serious side effects of the thiazide diuretics include hypercholesterolemia, and impaired glucose tolerance with consequent increased risk of developing Diabetes mellitus type 2. The thiazide diuretics also deplete circulating potassium unless combined with a potassium-sparing diuretic or supplemental potassium. On this basis, the consensus recommendations to prefer use of thiazides as first line treatment for essential hypertension have been repeatedly and strongly questioned. However as the Merck Manual of Geriatrics notes, "thiazide-type diuretics are especially safe and effective in the elderly."
Current UK guidelines suggest starting patients over the age of 55 years and all those of African/Afrocaribbean ethnicity firstly on calcium channel blockers or thiazide diuretics, whilst younger patients of other ethnic groups should be started on ACE-inhibitors. Subsequently if dual therapy is required to use ACE-inhibitor in combination with either a calcium channel blocker or a (thiazide) diuretic. Triple therapy is then of all three groups and should the need arise then to add in a fourth agent, to consider either a further diuretic (eg spironolactone or furosemide), an alpha-blocker or a beta-blocker. Prior to the demotion of beta-blockers as first line agents, the UK sequence of combination therapy used the first letter of the drug classes and was known as the "ABCD rule".
